The drivers of influenza vaccination in adults: Insights from a national Australian survey
Social scientists from the National Vaccination Insights Project, surveyed a nationally representative group of 2,009 adults over 18 years of age to understand what motivates them to receive the recommended influenza (flu) vaccine1 and compare findings to 2024 data collection.2 This survey was led by the Social and Behavioural Insights in Immunisation (SABII) research group.
The team has conducted in-depth interviews with adults over 18 years of age to further understand the vaccination motivators and barriers identified in the survey. The interviews are currently being analysed, and results are expected in 2026.
More information at the NCIRS page: Key Findings Summary
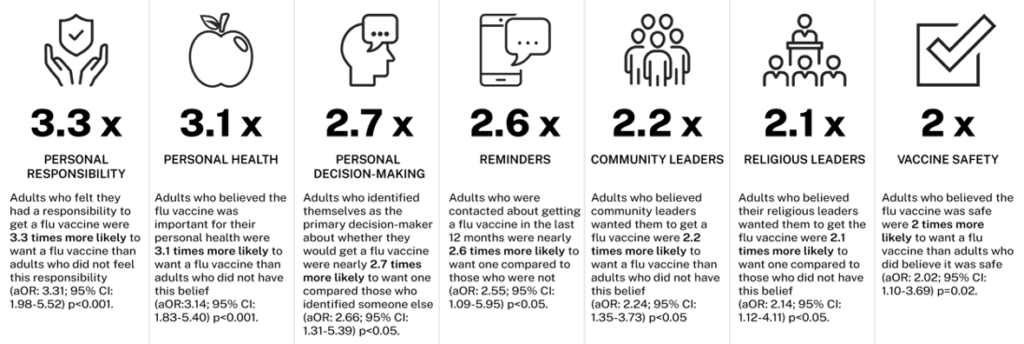
Researchers administered questions from an adapted version of the World Health Organization’s Behavioural and Social Drivers (BeSD) of vaccination survey to understand the drivers of adult flu vaccination. The following motivators were identified as influential in 2025:
Researchers also compared findings to last year’s survey:
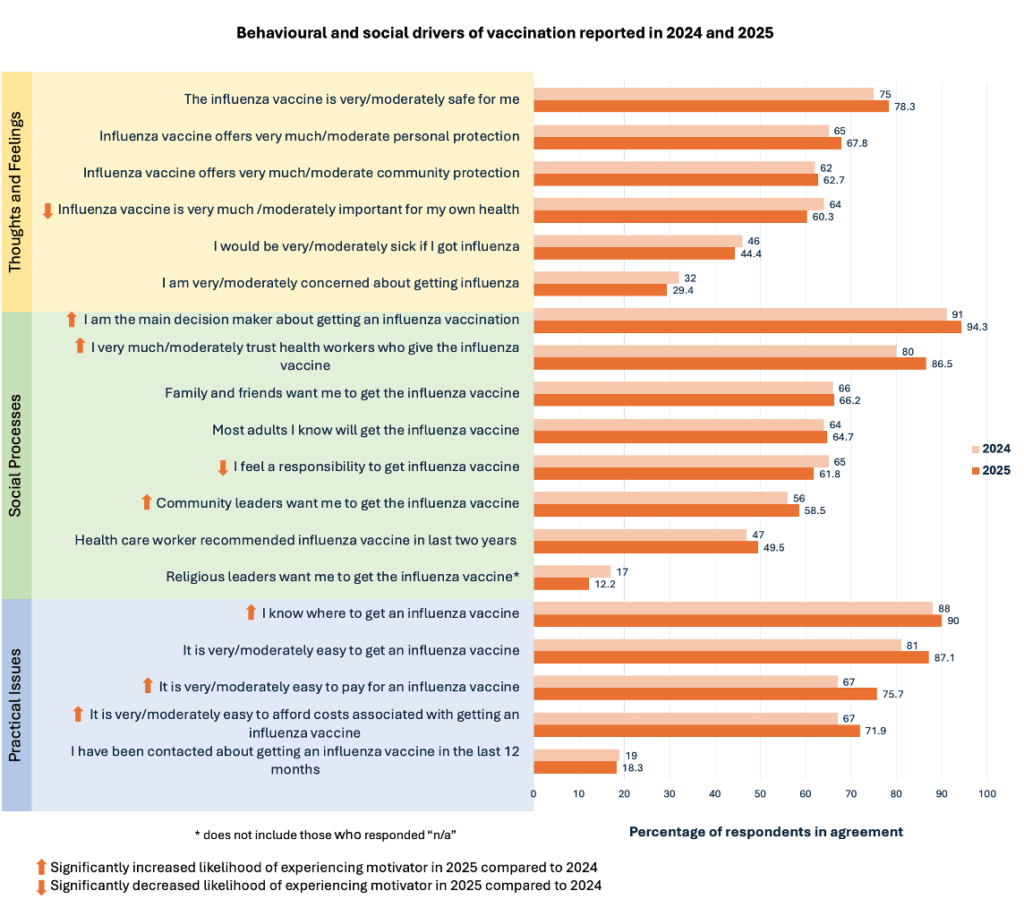
The likelihood of experiencing the following motivators changed between 2024 and 2025:
- Personal decision-making: In 2025, adults were 1.7x more likely to be the main decision-maker about whether to get the flu vaccine compared to 2024 (OR = 1.72, 95% CI: 1.36–2.19, p < 0.001).
- Trust in health workers: In 2025, adults were nearly 1.6x more likely to trust the health workers who give the flu vaccine compared to 2024 (OR = 1.58, 95% CI: 1.34–1.87, p < 0.001).
- Costs: In 2025, adults were 1.5x more likely to find it easy to pay for a flu vaccine (OR = 1.53, 95% CI: 1.33–1.75, p < 0.001) and nearly 1.3x more likely to afford the costs associated with getting a flu vaccine (OR = 1.26, 95% CI: 1.10–1.44, p = 0.001) compared to 2024.
- Access: In 2025, adults were nearly 1.3x more likely to know where to go to get a flu vaccination compared to 2024 (OR = 1.26, 95% CI: 1.04–1.54, p = 0.020).
- Community leaders: In 2025, adults were 1.5x more likely to report that community leaders want them to get the flu vaccine compared to 2024 (OR = 1.52, 95% CI: 1.22–1.89, p < 0.001).
- Personal responsibility: In 2025, adults were 15% less likely to feel a responsibility to get the flu vaccine in compared to 2024 (OR = 0.85, 95% CI: 0.75–0.99 p =0.035)
- Personal health: In 2025, adults were 15% less likely to believe that the flu vaccine is important for their health compared to 2024 (OR = 0.85, 95% CI: 0.75–0.97, p =0.012).
aOR=adjusted odds ratio; CI=confidence interval; P=p-value; OR=odds ratio.
Researchers asked people who did not plan to get the flu vaccine in 2025 why they had made that choice. A total of 368 people shared 409 reasons, which the researchers grouped into six main themes:
- Beliefs about personal health: Some adults felt they didn’t need the flu vaccine because they rarely get sick, had avoided flu in the past without it, or believed they were healthy enough to fight it off. Others thought they weren’t in a high-risk group, and a few said they might change their mind in the future if their health situation changes.
- Beliefs about vaccines: Some adults were concerned about vaccine safety and effectiveness. Many of these reasons were related to negative personal experiences with vaccination or concerns that began during the COVID-19 pandemic.
- Decision-making influenced by other relationships: For some adults, making a personal choice to get a flu vaccine was important and this was influenced by the way they viewed governments and health authorities. Some people were put-off by feeling pressured to get vaccines during the COVID-19 pandemic and others felt that they did not trust pharmaceutical companies, and those who promote vaccination.
- Vaccination processes and experiences: A small group of adults decided not to have a flu vaccination because they avoid needles. Some people gave other practical reasons, like the cost of the vaccine, being too busy, and finding it hard to book a convenient time
- Beliefs about the flu: A small group of people though that the flu is not a severe illness and would not make them sick. An even smaller group did not think that the flu could be spread in warm climates, so they did not need a flu vaccine.
- Medical reasons: A very small number of people said that they had allergies or health conditions that did not allow them to have a flu vaccine, or that their doctor recommended that they avoid it.
References
1. Christou-Ergos M, Sabahelzain MM, Steffens M, Kaufman J, Bolsewicz K, Danchin M & Leask J . Tracking the Behavioural and Social Drivers of Adult Influenza Vaccination: Insights from Australia’s First Serial Survey (August 11, 2025). http://dx.doi.org/10.2139/ssrn.5425394
2. Christou-Ergos M, Sabahelzain MM, Steffens M, Kaufman J, Bolsewicz K, Danchin M & Leask J. The drivers of influenza vaccination in adults: insights from a national Australian survey. Vaccine: X 2025. doi: http://dx.doi.org/10.1016/j.jvacx.2025.100683
