Several members of the SABII team attended the CDIC (Communicable Diseases and Immunisation Conference) on Kaurna country/Adelaide last week.
Julie Leask co-hosted a symposium with Katie Atwell titled, What Happens When Government Wipes its Hands of Vaccination?

The symposium explored global examples of how governments build and maintain vaccination uptake. They walked through what is already occurring and likely to unfold in the United States and beyond. Bringing together concepts from public health and political science with examples from a range of countries, Professors Attwell and Leask provided a comprehensive “state of the nation” for immunisation uptake.
Following their discussion, they were joined by panelists from government, research, and practice. The panel discussed the implications of the US situation for policy and programs in Australia and elsewhere, and what is needed to shore up government support for vaccination.
Speakers: 1. Professor Katie Attwell – University of Western Australia; Professor Julie Leask – University of Sydney; Professor Mark Jit – Chair of the Department of Global and Environmental Health, NYU; Professor Nicola Spurrier – South Australian Chief Public Health Officer; Ken Griffin – CEO, Australian Primary Health Care Nurses Association
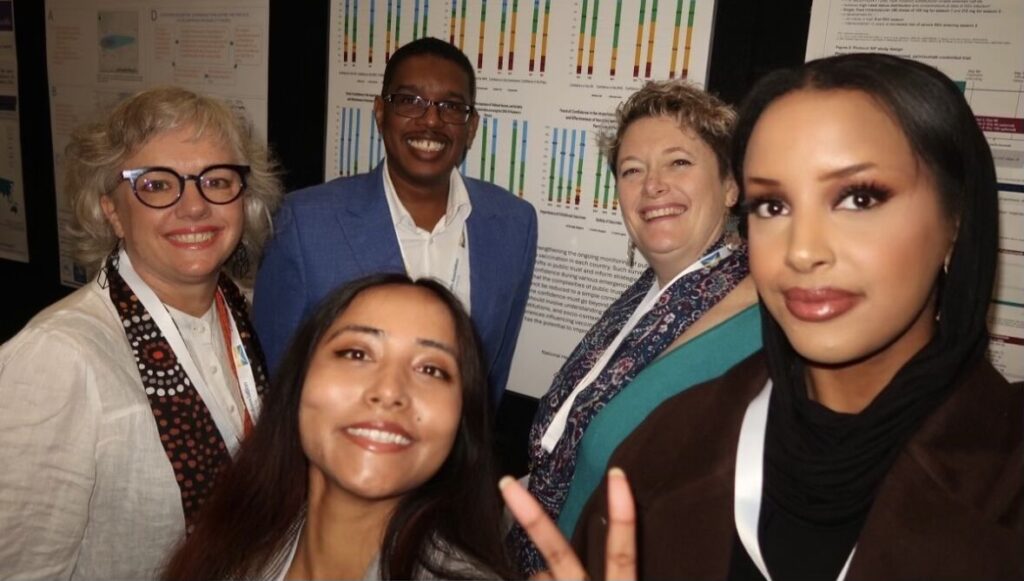
Other members of the SABII team, Ikram, Majdi, Kerrie, Rebika and Maria, also presented their work at the conference.
The theme of this year’s conference was ‘Future directions for immunisation and communicable disease control: embracing ideas, innovations and improvements’.
Well done to our SABII members for presenting their engaging and important work on the behavioural and social drivers of vaccination.